The Status (and Reflections) of the Pandemic with Dr. Fauci
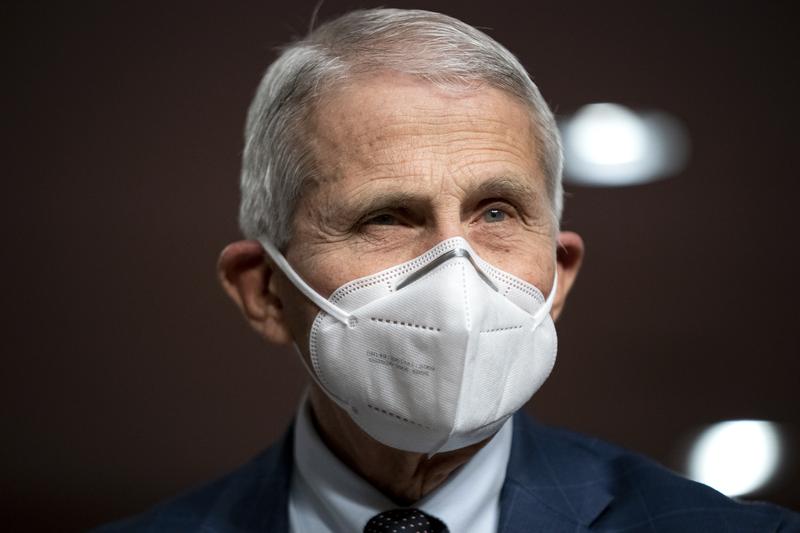
( Greg Nash/Pool via AP )
[music]
Brian Lehrer: Brian Lehrer on WNYC, and now we're very pleased to have a few minutes one more time before he retires with Dr. Anthony Fauci, who is about to close the book on his 38 years as director of the National Institute of Allergy and Infectious Diseases and leave his post as Chief Medical Advisor to President Biden. I got to speak with Dr. Fauci near the beginning of the pandemic in 2020, both about the virus and about his Brooklyn roots, and we're grateful he has made the time for us this week to share some thoughts on the state of COVID now and his life's work in pursuit of public health generally. Dr. Fauci, thanks so much for the time today. Welcome back to WNYC.
Dr. Anthony Fauci: Thank you very much. It's a pleasure to be with you. Thank you for having me.
Brian Lehrer: To begin on the news, I saw that you spoke this week about a couple of new Omicron variants called BQ.1 and BQ.1.1 that you're concerned about because of how they're spreading. Do you think we're about to see another surge like happened last winter with the original Omicron?
Dr. Anthony Fauci: Well, I think it's going to be inevitable that we'll see these new variants become more and more dominant because they seem to have a bit of a transmission advantage. They are getting greater and greater of a percentage of the isolates. It's a bit problematic in that some of them allude or escape the effects of some of the monoclonal antibodies that are given both to prevent infection in immune-compromised people such as those who have had organ transplantations, and some of them even allude the effect of the monoclonal antibodies that are used for treatment.
However, somewhat encouraging is that these variants, although they are different a bit from the BA.5 variant, which is the variant that the updated Bivalent boosters directed against, namely the one that we've just, over the last month or so, made available. That those variants likely would still have some pretty good cross-protection by the vaccine-induced immune response that we would hope more and more people do come in and get their updated bivalent B.5 boosts cause that could protect them.
An answer to your specific question, we can mitigate a bit any effect of what you would call a surge if we do some fundamental things like get more and more people vaccinated who have not been vaccinated, and if you've been vaccinated, by all means, get your updated booster. Because the difference in severe disease leading to hospitalization and death in people who are unvaccinated versus vaccinated, or even people who are vaccinated and not boosted compared to people who are vaccinated and boosted.
The protection against severe disease is extraordinarily better among those who've been vaccinated and boosted. It just makes plain common sense that if we're worried and concerned about a surge as we enter into the cooler months of the fall and the winter, that we all go out and get vaccinated. That really is the best thing that we could do as a society.
Brian Lehrer: What about other kinds of protective behaviors? I think we're in this very awkward situation now, Dr. Fauci, for people's personal decision-making where the death rate is not nearly what it was. It was like 2000 a day at the beginning of this year, but it's still shockingly high at around 300-something to 400-something deaths a day as a floor that were not falling below, and it looks like there's not much short-term prospect of going down from there.
I think every listener if they're not elderly or immunocompromised themselves, has those people in their lives, people who we really don't want to catch the virus at all, even if vaxed and with the treatments we have, but most people don't want to wear masks forever when we visit grandma or consider Thanksgiving a big risky thing again next month. Do you have advice for navigating the near and medium term, even after people have gotten vaxxed?
Dr. Anthony Fauci: Yes, there are several things you can do and I think one of the things that we want to make sure people are aware of, particularly as you get into the holiday season, as we approach Thanksgiving and Halloween and holidays like that, is that you can get tested and know literally within 10 or 15 minutes whether you're infected, or at least if you have enough virus in your nasal pharynx that you might infect someone else.
If you are going to have a gathering, particularly if that gathering includes the elderly and those with underlying conditions, it's not a big stretch to be able to get people to the day of the gathering, maybe several hours before, to do one of those antigen tests, and if someone is positive to not be part of the gathering. You can prevent these many outbreaks associated with dinners or parties or celebrations. That's one very easy way to do it.
Another way is that if you are in a situation where you have in your home or close to you a vulnerable person, you might go the extra mile and if you go into an indoor congregate setting where you're not sure of what the vaccination status of most of the people in the room are to wear a mask. I'm not saying mandating a mask because whenever you say mandate something that's like radioactive to people. I'm talking about common sense that's commensurate with the risk that you're willing to take.
If I'm somebody that has an elderly grandparent or parent at home, or someone who's on chemotherapy for cancer, besides getting vaccinated and boosted, I would do something extra and that would be wear a mask in a congregate indoor setting, and test myself intermittently so that I don't inadvertently bring home an infection, even if I am infected but I have no symptoms.
Brian Lehrer: You got COVID this year and took Paxlovid as a lot of people have seen on the news, then had a rebound case and took Paxlovid again. From what I've read and I've read that you're better and you don't have long COVID. If that's true, that's great.
Dr. Anthony Fauci: That is true.
Brian Lehrer: What do you say to listeners who may have asked themselves, how can Dr. Fauci get COVID? He's the ultimate expert on how to protect yourself. Was there something you didn't know or risks that you decided to consciously take?
Dr. Anthony Fauci: Well, I think it's just the manifestation of what the reality is that vaccines and boosters clearly protect you against severity of disease so that you might get infected, but it is highly unlikely that you will get severe enough disease to result in hospitalizations and God forbid, death. You superpose upon that, that if you do get infected, that we have very good antiviral drugs like Paxlovid, which are extremely effective in preventing you to get progression of disease leading to a serious consequence.
The fact that I got infected, that doesn't mean that I'm not trying to protect myself. It means that I didn't wear a mask 100% of the time, and there was some circumstances where it was very difficult to be wearing a mask, and that is likely the situation that led to my getting infected.
Brian Lehrer: People have to make these decisions for themselves about how much to "live their lives."
Dr. Anthony Fauci: Exactly, and I did that. At the time I got infected was several months ago in June of this year, 2022, and I went to a social function in which I came into it with a mask, but when I started seeing some old friends, for a short period of time, I took my mask off. I took a risk, I took a chance, and I paid for it because I got infected. Luckily, I did not get a severe infection, and luckily, I had the availability of Paxlovid, which made it a relatively uneventful infection for me.
Brian Lehrer: I want to ask a few questions about your 50-plus-year career in public health and over that period of time, what would you say are the biggest advances that science has made in your field of infectious diseases?
Dr. Anthony Fauci: Well, they're pretty obvious. Ones that is not only one of the biggest advances in infectious diseases but maybe one of the greatest advances in all of medicine. That is the development of a combination of antiretroviral drugs for HIV infection that has converted that disease from a universally or almost universally fatal disease to one where people who, if they get treated early with appropriate combinations of drugs, can lead essentially almost a normal healthy lifespan.
That is, historically, one of the greatest advances that have been made in all of medicine, not only infectious diseases. Then there are also other advances that have been made in my field, for example, vaccines against diseases like [unintelligible 00:10:59], hepatitis, human papillomavirus. Those vaccines have saved many lives and I could go on and on. There have been a number of very important advances in my field.
Brian Lehrer: What do you consider some of the next goals and next frontiers?
Dr. Anthony Fauci: Obviously, one of the holy grails of infectious diseases that we have not accomplished yet is to develop a safe and effective vaccine against HIV. We're making considerable and progressive progress, but we're not there yet. That's one unmet goal. The other is, if you look at the big killers of infectious diseases, it's malaria and tuberculosis among other globally important infections.
I would like one day to see good preventions either vaccines or MONOCLONAL antibodies against malaria, which kills over 600,000 people a year, mostly babies in Southern Africa. We have got to do better than that. One of the ways is to get a highly effective vaccine. That's another unmet goal, as well as better treatments and prevention in the form of a vaccine for tuberculosis. Because if you look at the major global killers, it's HIV, tuberculosis, and malaria among several other infections.
Brian Lehrer: I went to grad school for public health. I don't know if you knew that. It has informed my approach to every subject that I cover in journalism and public health, to me, is largely about social justice, people who are affluent enough will have the luxury of making changes to their behaviors or their surroundings. One science informs them of the threats to their health or develops the treatments and preventive vaccines and other things you were just describing. For the non-affluent, public policy is also needed to protect them to any similar degree. I wonder how much you see public health that way.
Dr. Anthony Fauci: Oh, absolutely. I think you are absolutely correct on that. We have a responsibility, I have always felt that way. That is almost, and it is a moral responsibility if you are living in a rich country that has resources is to do whatever you can to make available to those who are less fortunate in low or middle-income countries. Interventions be they prevention or treatment that are easily available in the developed world.
Try as best as you can as a public health policy to undertake the responsibility to get those interventions for people whose lives can be saved if they nearly had access. One of the classical and historic examples of that, and I feel enormously privileged to have had the opportunity to be a part of that, was during the presidency of George W. Bush when he felt strongly given the fact that we had such effective therapies for HIV.
People in the developing world, particularly Southern Africa, among other regions, were dying of a disease that we had treatments for, merely because they didn't have access to treatment, prevention or care. He tasked me to be one of the architects of the PEPFAR program, the president's emergency plan for AIDS relief which provided billions and billions of dollars to provide drugs and prevention and care in the developing world. That program, which we started in 2003, has been responsible for saving now 20 million lives. I think that program that was championed by President Bush is a classic example of what you're talking about global health and the responsibilities we have to get equity in global health.
Brian Lehrer: Last question. What are your plans for retirement? Are you going to write a book or anything? Are you going to go back to playing stickball on the streets of Dyker Heights? What do you have in mind?
Dr. Anthony Fauci: I wish I was able to play stickball again, but I might try that. To be honest with you, I haven't made any definitive plans because as part of the ethical rules, while I'm still director of a large institute, I have to wait until I actually step down before I can start negotiating. I will be doing a lot of writing and lecturing and perhaps even write a book. I'm not sure yet. I certainly am not going to retire in the classic sense of retiring.
Brian Lehrer: About to retire in the official sense at least as director of the National Institute of Allergy and Infectious Diseases after 38 years as director and leave his post as Chief Medical Advisor to President Biden, but as we hear, remain active in the field of public health. We thank Dr. Anthony Fauci for your service to our country all these years. Thanks for coming on to talk to the WNYC listeners one more time. Good luck, whatever you do.
Dr. Anthony Fauci: Thank you very much. My pleasure to be with you. Thank you for having me.
Copyright © 2022 New York Public Radio. All rights reserved. Visit our website terms of use at www.wnyc.org for further information.
New York Public Radio transcripts are created on a rush deadline, often by contractors. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of New York Public Radio’s programming is the audio record.

