COVID-19 and the City
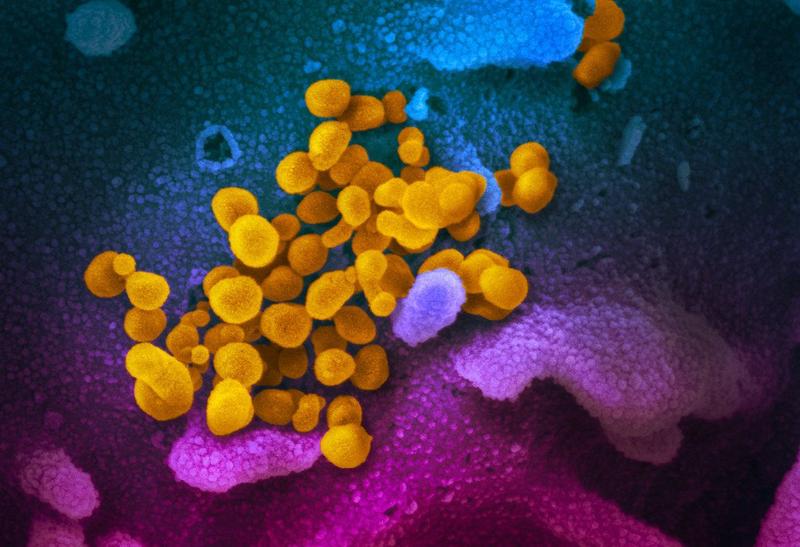
( NIAID-RML )
[music]
Brian Lehrer: It's the Brian Lehrer show on WNYC good morning, everyone. We're all now searching for that place between prudence and panic on Coronavirus, aren't we? We're searching for it as individuals deciding how much to avoid crowds, avoid every doorknob, how necessary is it to wash our hands after every time we use our phones away from home? Should that couple you know still have their 200 person wedding reception? Should you no longer attend? We're searching for the answers as individuals and institutions are searching for answers too.
Columbia University maybe you heard this morning is closed today after one member of the Columbia University community is under quarantine after being exposed to the virus. Scarsdale public schools are closed after one middle school faculty member tested positive. South by Southwest the big festival that happens in Austin every year is canceled. Yeshiva University played a college basketball playoff game in Baltimore, with fans prohibited because of the earlier Yeshiva student case son of the lawyer from Westchester who got the virus. Here's Governor Cuomo speaking yesterday.
Governor Andrew Cuomo: What happened in Westchester County is a person who was positive was in a very large gathering and people then got infected and then they went to very large gatherings so that is my point about the density. An infected person in a large gathering can infect many people quickly that's what we're seeing in Westchester. That's why we want to avoid large gatherings we want to avoid density, that's why I'm reaching out to the private sector companies. By the way, also local governments, I'm asking them to stagger their workforce, that's why I'm asking citizens to stay home, telecommute when you're on public transportation, find the least dense car or bus available because it is the density it is the gathering.
Brian: Governor Cuomo at a news conference yesterday suggesting those behavior changes, but he says that that prudence need not lead to alarm, especially with zero deaths so far in the state and only eight hospitalizations.
Cuomo: If people understand the facts here, they shouldn't be alarmed. The fear and the anxiety is greatly outpacing the reality and we're fighting the fear even more than the virus, frankly.
Brian: Cuomo on MSNBC with Alex Witt here's more.
Cuomo: The data, Alex, should calm people yes we have 105 cases only eight people are in the hospital. Johns Hopkins has been tracing all the coronavirus cases, over 100,000 60,000 people have already recovered just about 40,000 are still ill. Number of fatalities, 3000 out of 107,000 cases so it's avoiding the massive disruption, it's protecting those vulnerable populations, and that's why we tried to contain How do you contain? You test, you test, you test, you test you find the positive person you isolate them.
Brian: Let's talk about where we are happy to have with us Dr. Jessica Justman Professor of Medicine in epidemiology at Columbia University and an attending physician in the Division of infectious diseases at the Columbia University Irving Medical Center. She is also Senior Technical Director at ICAP a Global Health Center at the Mailman School of Public Health at Columbia. Dr. Justman, thank you so much for joining us welcome to WNYC.
Dr. Jessica Justman: Good morning and thank you.
Brian: Listeners, we can take your Coronavirus questions for Columbia epidemiologist Dr. Jesisca Justman, an epidemiologist is someone who studies the spread and control of diseases in populations. Our phone number 212-433 WNYC 433-9692. Dr. Justman, I want to start with that last thing the governor referred to, you test, you test, you test, you find the positive person you isolate them. There's a lot of unhappiness over the availability of tests and the allowable types of tests right now. Does our area have what it needs?
Dr. Jessica: Yes, our area does have what it needs now, and testing is going to be increasingly available in fact, as the week goes along. There were some initial technical glitches with the test kits and I think that access to testing was more limited than perhaps we might have wished, but people have been working very hard and really doing their best and I think that we are now in a much better situation. New York state provides testing at the Wadsworth lab in Albany. A number of hospitals, including Columbia University, as of today, have the capacity to do the testing and commercial labs now have the capacity to do the testing.
I think we're going to see that really open up and as that happens, more and more people will get tested, we will find more cases and I think we should all be prepared for that number to really increase dramatically and we shouldn't be surprised or put off by that when that happens. Those cases are out there they just need to be identified and then all of the appropriate measures can follow after that happens.
Brian: When you refeed just now to the private labs, here's the governor again asking for two things he says we're not getting from Washington.
Cuomo: Find the positives, quarantine the positives, contain it the best you can because if you have to do a massive close down like China, like Italy, that's going to hurt this nation's economy. It'll hurt the state, but it's going to be a national phenomenon.
Brian: Sorry, that's not the clip I thought it was but he said we're not having the ability that we need to have the private labs do testing, not just government labs, and also something he called automated testing. I'd like to know since I think we're hearing that term automated tests from the governor a lot what are those?
Dr. Jessica: Automated tests are not going to be just specific to Coronavirus testing, there's all kinds of testing that's done that's automated that allows for a large number of tests to be done rapidly. That means that you don't need to have a lab staff member work on each particular test tube one at a time but you can do hundreds at a time that's what automated testing would mean. Sometimes you'll hear the term high throughput, and that would mean the same thing.
Brian: Is the federal government somehow serving as an obstacle to be able to do that in New York do you know?
Dr. Jessica: I really don't think that's the case at all and again, the commercial labs now this week are able to provide testing. The Food and Drug Administration a few weeks ago issued an emergency use authorization to make it easier for labs including commercial labs, to roll out the testing.
Brian: When he says and you say, isolate those who test positive, the Yeshiva University case, with one student not on the basketball team positive and they closed the playoff game to fans to be prudent. Your school of Columbia University is shut for someone being quarantined because they were simply exposed to someone with a virus. We don't know as I understand it, if the one Columbia person is even positive, the South by Southwest festival canceled as I mentioned, just out of total prevention. Can you explain the standards for when to close what and if you think institutions are getting it about right?
Dr. Jessica: Sure just to clarify, at least as of last evening, the Columbia University person was not considered a case, was not positive, but is on quarantine so I just wanted to make that clear.
Brian: Which is what I said and that's part of my question really is, here's a case where somebody was merely exposed to somebody who had been positive, and as you say, is on quarantine without being the case in this person's own right. Yet, all Columbia University is closed today so explain the rationale and how that fits into a larger strategy?
Dr. Jessica: Sure, I think going back to your early earlier question, there aren't any universal standards that provide clear guidance on when to close events or cartel events and I think it really requires the use of judgment from public health experts and other experts. I think that's perhaps not very satisfying it would be nice to know that there were carved in stone guidelines and standards. At the end of the day, we all have to do our best job and use our judgment. I think it's a matter of saying that perhaps if there's one case at the university or in another setting that requires quarantine, there are perhaps many others that are at this moment in time unknown and undetected. The prudent thing to do is to be more conservative. That would be the way I would look at it.
Brian: Before we take some phone calls, I want to switch more to the personal decision side now. The Centers for Disease Control website now includes a page that says, "If you are at higher risk for getting very sick from COVID-19, you should avoid crowds as much as possible. When you go out in public, limit close contact and wash your hands often." That's the exact wording on the site. If you're at higher risk for getting very sick from COVID-19, you should avoid crowds as much as possible and the other language. Then it says, "Who is at higher risk?"
It answers that question with the words older adults as one category, and it adds people who have serious chronic medical conditions like heart disease, diabetes, and lung disease. As for what age they mean by older adults, I don't see it on the CDC site. CNN quotes Dr. William Schaffner, an infectious disease specialist at Vanderbilt University and longtime advisor to the CDC, William Schaffner, not the guy from Star Trek, saying, "Anyone over 60 in addition to those with the serious chronic health conditions should strongly consider avoiding crowds, even including family events and religious services." That's a quote from Dr. Schaffner.
I think this all has a lot of people confused about how risk-averse to be in their own lives. For example, if you're healthy, but over 60, how do you understand it?
Dr. Jessica: I think that there isn't a one-size-fits-all solution or interpretation to this guidance. Each person has to think about who you are, and where you are, and really, I would say, who's in your social network. Different people who are the same particular age are different, sometimes we say biological ages. Some people who are 60 are very fragile and have many chronic health conditions and others are not. I think, again, it's really not possible to have a one-size-fits-all interpretation to this type of thing. I'm sure that CDC thought long and hard about how to phrase this and decided not to use a particular age band in their guidance.
I know Dr. Schaffner, I respect him. I understand that people do want to have a particular age to keep in mind. I think it's something as a approximate guidance, but everybody should interpret it and decide for themselves what their health is and also what the health is of the people that they spend a lot of time with at home or in other social circumstance.
Brian: The Cuomo clip we played at the beginning, it sounds like he's basically telling everybody to avoid crowds if we can, to telecommute to work if we can, to avoid densely crowded subway cars, maybe wait for the next train and hope that the next train has cars that are less crowded. That's pretty universal.
Dr. Jessica: That is part of a term in epidemiology we use, it's called social distancing. That is known to be a mitigation approach, which will reduce the severity of an epidemic and really should then also minimize economic, and political, and social disruptions. I think it's also just good common sense. If you don't have to go to work at peak of rush hour, it's much better to go when things are less crowded.
Brian: With Dr. Jessica Justman Columbia University physician and epidemiologist. Jenny in Manhattan, you're on WNYC. Hello, Jenny.
Jenny: Thank you for taking my call. I was hoping that our expert here in the line now with us could help us understand a little bit more how this virus compares to, let's say, the flu or pneumonia. Until recently, there were no vaccines for flu and pneumonia. People weren't quarantined and told to stay home. People could catch flu from other people. Even with the vaccines these days, I understand that it only protects against certain strains and not other strains. You could still get the flu even having had the vaccine. I was wondering how that compares. In terms of contagion, even these days, people still get flu and pneumonia, people don't all get quarantined against those diseases. Could you help us understand that better?
Dr. Jessica: Hi, Jenny. I think that there are a number of similarities and a number of differences between ordinary influenza flu and coronavirus. They're both caused by viruses. They both can lead to pneumonia. They both have similar routes of transmission with respiratory droplets. I think a big difference is that with ordinary influenza flu, the percentage of people who die as a result of flu is much, much lower than what appears to be the fatality rate for coronavirus. In an ordinary year, influenza will be associated with deaths in 1/10th of 1%, 0.1%, and sometimes lower. We had a big outbreak of influenza 10 years ago.
We might have heard it referred to as H1N1. That was even a whole order of magnitude lower in terms of fatality 0.01%. By contrast, the coronavirus epidemic so far, the rates are much higher. Last week, the World Health Organization estimated the case fatality rate is 3.5%. You can just get a sense of-- That's 30 times higher. Many experts and I agree with this prediction as well, fell that 3.5% is not going to be what the ultimate fatality rate is going to be like. We think that it's going to become much lower as testing becomes more available and we understand the real scope, the extent of how many people have mild cases who are really doing fine.
I think a lot of it is about that difference in fatality rate. Going back 100 years ago to the Spanish flu, which a lot of people are talking about, at that time, supportive therapy was not nearly as effective as it is now. We have antibiotics for secondary infections. We have ventilators and very sophisticated approaches to supporting people while they have pneumonia. There's a lot of work going on to develop a vaccine and treatment for coronavirus. I'm optimistic that the fatality rate for coronavirus is going to go way down.
Brian: Jenny, thank you so much for your phone call and good questions. Let me follow up on Jenny's question in your answer by coming back to the question of individual behavior change and institutional change, like closing things. My understanding of the flu fatality numbers in this country, you could probably correct me if I'm off, from 35,000 to about 70,000 per year in flu season. We don't turn society inside out and upside down because of that very high number of deaths and yet we're doing it in this case in anticipation of a death rate that you say once all the numbers are in because we have a large enough sample, may turn out to be higher, but not that much higher.
How do you understand the recommendations for behavior change by individuals and institutions in comparison to the flu. Are we freaking out too much over this? Should we be doing more every year like this because of how deadly the flu is?
Dr. Jessica: I'm just trying to make sure that I'm understanding your question. You want to know if we should be doing more every year, given that we have flu and flu-related deaths.
Brian: So many flu-related deaths, or conversely, are we overreacting to this because it may not turn out to be any worse than a given flu season for which we don't turn society inside out?
Dr. Jessica: I think it's a good question. I'm going to say, I think that in terms of what's going on now, the number of school closures has been rather limited. I think that the amount of social distancing that's going on. To me, it makes sense. I think we're all worried there's, I think some have used the term, an info gimmick. There's so much information out there that it adds more to the panic side of the equation. I mean, you began the show talking about the contrast between prudence and panic and how to find the right balance. I think that's really the key question. I think perhaps there even might be more school closures coming.
In terms of our approach every year with ordinary flu more people could get vaccinated, and that would protect people, and even if you do get the flu, after having had the flu vaccine, the severity of illness will be reduced, and the chances of death would be reduced. From the point of view of vaccination for ordinary flu, we could still do more, there's still room to improve.
Brian: Yes. I guess another difference is there is a vaccine for the flu, although even with the availability of the vaccine, that many 10s of thousands of people a year die. I don't know if that's from just people not getting the vaccine, who should, and almost all those deaths could be prevented or a large percentage of them but this is different in at least that respect. There's not even the option of a vaccine at this point. Let's take another phone call and my guest is Dr. Jessica Justman epidemiologist and physician at Columbia University, Lisa in Westchester, you're on WNYC. Hello, Lisa.
Lisa Allison: Hi, thank you for taking my call, relates to something that was just said really, but how are we supposed to deal with this conflicting advice from experts. We read, for example, I read the other day and appeared in The New York Times regarding school closures that was really advocating quite strongly that it would be very helpful to close schools in order to stop the spread of virus based on evidence of other epidemics. Equally, the LA Times had an op-ed arguing the exact opposite, both from very well respected people who seem to use good evidence. I think that is creating a huge amount of unsettlement and panic amongst the public because you feel like you don't know who to trust, who to believe.
Brian: Yes, doctor, Justman. That's exactly where we are right now, isn't it?
Dr. Jessica: Yes. I think that you are really pointing out a very important area of tension and confusion. I think that it's, on the one hand, good to stay informed. Also at the same time, it's probably worth just being very careful and to consider who the source of the advice is coming from. I didn't see the piece in the LA paper. I don't know who wrote it or where the information is coming from. I think we're going to have to just keep an eye on what CDC is telling us to do, what New York City Department of Health is telling us to do, and then just taking our cues from there.
Brian: Lisa did you also tell us-
Lisa: We have schools closed. Scarsdale they have closed within where I live, and Marinette School District, there is a family quarantined and our school have decided not to close the children apparently don't have symptoms, but is that kind of thing that I think people find extremely disconcerting.
Brian: The lack of consistency?
Lisa: Yes.
Dr. Jessica: I think the other thing that's difficult, even beyond the lack of consistency is that the rapidity with which the news and various events emerged so that in the situation changes from the morning to the afternoon, if not hour by hour, and I completely understand how unsettling it is to have something that keeps changing and I think we have to remember that, you know, it's a new virus, it's a new infection. I think as humans, it's hard for us to deal with something that's completely new and different.
Brian: Lisa, I understand you told our screen also that you had a question about a particular person you know who's got-
Lisa: It is a very personal question. She'll be very upset that she should be asked the question, but I'm going to ask anyway, my 25-year-old daughter who actually is working and commuting, she has asthma well-controlled but she has had several bouts of pneumonia in her life, twice hospitalized, and I would really like her to stay home [laughs] and work from home and ask to work from home. There's been no directive from her place of work to do that, what would the advice be?
Dr. Jessica: I think for that situation, I would go along with Governor Cuomo's advice, which he really put in very simple and clear terms to try to commute when it's not so crowded and sit in an emptier car so that you have a little more distance from people. I think the thing to remember is that most of the cases that are transmitted among contact, they're happening among household contacts where you have more prolonged exposure to people who are going to be within four, five, or six feet of you, they don't appear to be as much related to casual contact.
In fact, I took a look at a paper earlier today, it's not been peer-reviewed, it's not been published, but it showed that even among household contacts, and this was in China, about 15% of household contacts were getting ill after exposure to a case. I have an optimistic interpretation of that. I think it's great that it's not 90% or even 50%, but it was 15% and that's, again, from household contacts with prolonged exposure.
Brian: Lisa, thank you very much for your call and good luck to you and your daughter. Let me follow up on that question about her daughter because asthma is a chronic condition that affects the lungs, obviously, and yet, I feel like I'm not seeing it on the list of chronic medical conditions for which people should be careful. I keep seeing heart disease, diabetes, and lung disease, maybe asthma is lung disease. You tell me, but what about for all those people with controlled asthma out there?
Dr. Jessica: I mean, yes, asthma's lung disease, and it is a lung condition that's associated with inflammation, certainly, when the Asthma is not well controlled. I think that it goes back to what I was saying before about it not really being one size fits all. I think somebody who's got very mild asthma that's under good control, their inflammation will be less, and probably their risk if they were to get infected with coronavirus would be similar to that of a jet person in the general population. For somebody with very severe asthma that's difficult to control, I think that's somebody who should perhaps take additional precautions.
Brian: Here's the federal government's leading infectious disease specialists, the widely respected Dr. Anthony Fauci asked on Fox News Sunday yesterday if the US needs to close off whole communities like Italy has done in their north.
Dr. Anthony Fauci: I don't think it would be as draconian as nobody in a nobody out, but they'll be if we continue to get cases like this, particularly at the community level, there will be what we call mitigation, where you'll have to do essentially, social distancing, keep people out of crowded places, take a look at seriousness, do you really need to travel those kinds of things. I think it's particularly important among the most vulnerable
Brian: What I'd like to ask you to do out of that clip, Dr. Justman is explain that term mitigation that Dr. Fauci used there because I'm hearing that referred to as what you have to do if containment isn't working well enough. What do we mean by containment and what do we mean by mitigation because I keep hearing those juxtaposed in the press.
Dr. Jessica: Sure they are really complementary terms. Typically at the beginning of an epidemic, containment measures are put into place. Classically, quarantine, and contact tracing. The idea of containment is trying to avoid the amplification of new cases at the very beginning stages of the epidemic. After the containment measures are put into place, then the mitigation approach typically follows. Of course, these things can be done almost simultaneously, but usually begin with containment. Mitigation, the easiest example to understand is social distancing with school closures, but the goal of containment is to avoid having new cases the goal of mitigation is to reduce the impact of the epidemic as much as possible. They are closely related concepts but there is a bit of a distinction.
Brian: Sheryl in Soho you're on WNYC, hi Sheryl.
Sheryl: Hi, thank you for squeezing me in. Have we learned yet if any part of the virus is seasonal and or heat-sensitive?
Brian: Thank you very much for that question. Yes, I'm sure a lot of people are wondering if like the seasonal flu this is going to abate at least until the fall once spring really comes.
Dr. Jessica: I think that the answer to that is maybe. We don't really know. There are reasons that we can be hopeful. The SARS epidemic from 2002 that tailed off in the month of July. Typical Influenza flu does have a seasonality. The reasons behind the seasonality are complex. Some of it might be due to people spending more time indoors, in gatherings, and sort of a higher density of those gatherings in the winter months, and then in the summer months, people spend more time outdoors.
Once you're outdoors you're in contact with surfaces that are exposed to ultraviolet light so that helps keep things clean. These diseases are spread through respiratory droplets and the droplets themselves appear to behave differently in different temperature and humidity conditions so that they can travel farther in colder drier conditions and we know that from some experiments with guinea pigs. It really might get much better, but the coronavirus infection that is called MERS, Middle Eastern Respiratory Syndrome, that took place primarily in Saudi Arabia and it is hot there. I don't think we can completely count on temperature and humidity to be the answer here and we just have to be prepared.
Brian: Let me take one more call for you and then listeners we're going to go on to another guest to talk more about the politics of the coronavirus right now both with the Trump administration and with the Democratic presidential hopefuls with six states voting tomorrow including Washington State which is of course, where the virus has been the most concentrated so far. I also want to tell all of you that I will be back tonight at seven o'clock for a one-hour call-in special here on WNYC specifically on coronavirus. We're going to do an extra show in the evening drawing together for a live and local WNYC call-in about coronavirus and what's happening in our area.
We'll hear more of the latest word from public health and safety officials and we'll take many of your phone calls. That's going to be tonight. A coronavirus call-in special at seven o'clock here on WNYC. Let's take one more phone call for Dr. Justman from Columbia. Louise and Hopewell Junction you're on WNYC hello Louise?
Louise: Hi, good morning so I'm an RN and I travel into Manhattan, mostly Harlem, the Bronx, and also Westchester. I do evaluations in patients' homes and our patients' are very high risk. They're usually chronically ill and they're elderly. I spend about two sometimes three hours at one time in their home and I think based on my past experience with infections control that I should-- if someone is sick, showing any signs of a fever or a sore throat or a cold because of the length of time that I spend in their house that I should put an N95 on me and perhaps a surgical mask on them.
I'm not being given that guidance and a lot of the RNs' who I work with and I'm not hearing anything about healthcare workers who work in the field. Who work out in the community and again I'm going into the home of people who are elderly, chronically ill multi-system involvement spending long periods of time in their home with direct contact with them, lots of time with them and also I'm in contact with their surfaces and I'm not hearing anything even from my own company surprisingly along those lines. What do you think?
Dr. Jessica: Is this a question about protecting yourself or about protecting the patients' that you're with?
Louise: Both because I'm going from one patient's home to another patient's home and I'm also going home to my home so there's a concentration of exposure potential.
Dr. Jessica: I think that if you're sick you have any symptoms, well you probably shouldn't be going to see patients, but I think that would be a reasonable time to wear a mask to protect others. If you're taking care of people who are ill in my opinion, I think that it's reasonable for you to wear a mask. You can begin to sort this depending on the exposure of the person that you're seeing.
If you're seeing a homebound elder who doesn't go anywhere and he doesn't have anybody else visiting him/her, I think you'd probably agree with me that that person is going to be very unlikely to have coronavirus but might have flu or other type of common cold. If you're seeing somebody who you think has had some kind of exposure, it would make sense for you to protect yourself with an N95 mask and to help that person seek attention and get testing.
Brian: Louise, I hope that helps, and certainly every institution that employs people like Louise needs to come up with some kind of policy. She says she's not getting guidance from her employer. Hopefully, that will change for her very soon and everybody out there who is involved in running any kind of health organization. I'm sure you are dealing with this and if you're not you need to deal with it to protect healthcare workers who are among the most vulnerable and the most exposed as well as their own patients. Before you go just one last question?
You've worked around the world as I understand it on global infectious disease issues. Have you ever seen anything like this? Northern Italy now, Venus, Milan all around there pretty much locking down like China did in Wuhan. Movie theatres telling people not to go to, to religious services even just extreme measures like I don't remember ever seeing in response to anything. Have you ever seen anything like this?
Dr. Jessica: I haven't seen anything like this that is unfolding at this particular pace. A lot of my work involves the HIV epidemic which is very extensive but that unfolded at a slower pace, but a very still dramatic epidemic and one at the beginning was uniformly fatal. Many aspects of it certainly were different. Neither you or I are-- really our listeners were around during the Spanish flu. My senses that it was very similar to what we're experiencing now and even more dramatic because we just didn't have the kind of supportive care then that we have now.
Brian: Dr. Jessica Justman is a professor of medicine in epidemiology at Columbia University and an attending physician in the division of infectious diseases at the Columbia University Irving Medical Center. She is also a senior technical director at ICAP a global health center at the Mailman School of Public Health at Columbia. Thank you so much for lending your time and expertise.
Dr. Jessica: Absolutely my pleasure. Thank you.
Copyright © 2020 New York Public Radio. All rights reserved. Visit our website terms of use at www.wnyc.org for further information.
New York Public Radio transcripts are created on a rush deadline, often by contractors. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of New York Public Radio’s programming is the audio record.

