The Nobel Prize for Understanding Autoimmune Disease
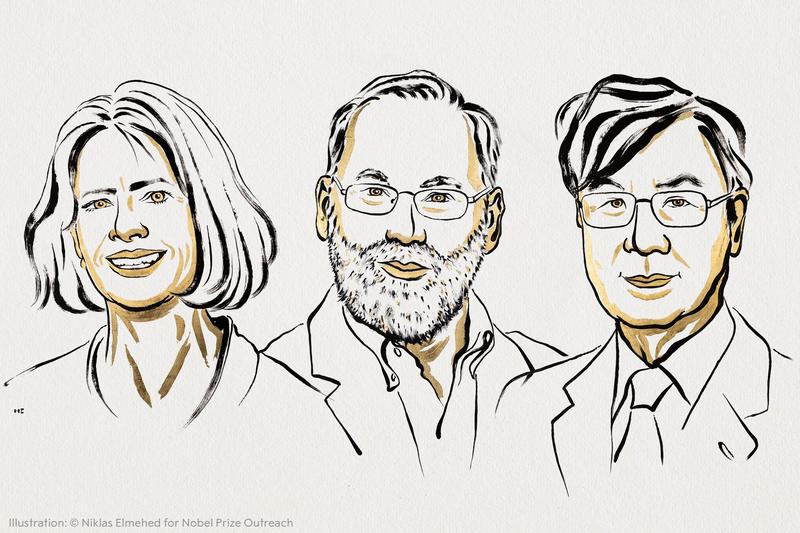
( Ill. Niklas Elmehed © Nobel Prize Outreach / courtesy of The Nobel Prize )
[music]
Brian Lehrer: It's the Brian Lehrer Show on WNYC. Good morning again, everyone. Today, for our Health and Climate Tuesday section of the show, which we do every week, we're going to be on the health side. This is the week the Nobel Prizes are awarded. Will President Trump's dream for the peace prize come true on Friday is the thing that most of the media are focusing on. Of course, we'll have to wait till Friday to find out. We will cover the Nobel Peace Prize winner, whoever it is, on Friday's show.
In case you're interested, by the way, the website Sportsbook Review looked at various betting sites and concluded that the favorite for the Nobel Peace Prize is Yulia Navalnaya, widow of Russian opposition leader Alexei Navalny, who wound up in prison and then dead in prison on Vladimir Putin's watch. Sportsbook Review says Yulia Navalnaya is seen as having about a 34% chance of winning the peace prize. Guess what? Trump is right behind with 32% betting odds.
Behind them, and also seen as in the running are Volodymyr Zelenskyy, UN Secretary General Antonio Guterres, activist Greta Thunberg, NATO as an organization, and Chef Jose Andres, founder of the hunger relief organization World Central Kitchen, which, as many of you know, lost seven of its workers in an Israeli drone attack in the war in Gaza. I don't know if anyone actually bets on Nobel Peace Prizes, but the books do put out the odds. We will know the answer to that on Friday. Maybe some of you will have won or lost money on the Nobel Peace Prize winner.
Yesterday, three scientists, Mary Brunkow from Seattle, Fred Ramsdell from San Francisco, and Shimon Sakaguchi, if I'm saying that right, of Osaka, Japan, received the prize in physiology or medicine. This is the Nobel Prize in physiology or medicine "for their discoveries concerning peripheral immune tolerance," which has to do with what stops the body's immune system from attacking itself and why, when it doesn't work, we get an autoimmune disease. Now, lately, as I don't have to tell you, the science of immunology has taken a beating under HHS Secretary RFK Jr., especially as it relates to immunizations, vaccines.
Let's spend some time to understand this prize for this scientific discovery in that field. I wonder if celebrating immunology at this particular moment had anything to do with the politics. I'm joined for this, once again, by Dr. Daniel Griffin, MD, PhD, Chief of Infectious Disease Medicine for Island Infectious Diseases on Long Island, a clinical instructor of medicine at Columbia University, president of the group Parasites Without Borders, which provides information to medical professionals in countries where parasites are a major cause of disease. He is co-host of the podcast This Week in Virology, or TWiV, as they call it. Dr. Griffin, always great to have you. Welcome back to WNYC.
Dr. Daniel Griffin: Thank you, Brian. Thank you for having me. Exciting to be on for this Nobel Prize discussion.
Brian Lehrer: Before we even discuss the discoveries, do you in the public health community have betting odds for the Nobel Prize in medicine, or do you think that's just a Peace Prize thing?
Dr. Daniel Griffin: I think it must be a Peace Prize thing. I was listening to that and wondering. No, we do not actually bet on this. We gamble in other ways, I guess. [chuckles]
Brian Lehrer: [chuckles] Yes, right. My head is spinning thinking of ways that infectious disease specialists have to gamble. This award goes to research into the immune system around T cells, I see. Thanks to COVID, probably many more of us than did before have some ideas of what T cells are versus B cells. Maybe you can give us a quick lesson in what T cells are.
Dr. Daniel Griffin: Sure, sure. I'm glad to be on to discuss this. You're forcing me to bring out my very nerdy side, which is a PhD in immunology. Just to give people an overview, because I think that we have learned a lot, actually, about the immune system during COVID. We learned about those antibodies that are made by certain immune cells called B cells. B cells do other things, by the way, but we also learned about T cells, and T cells are these immune cells that we realize are really important when we get infected by a virus, helping us clear that virus, helping us from getting severe disease.
A lot of discussions with those vaccines and actually prior infection, like did we get good memory T cells to protect us in the future? Good memory B cells to make antibodies for the future. One of the dark side of our immune system is sometimes it can turn against us. Sometimes those B cells might make antibodies, the autoantibodies, that start binding and targeting our own organs. T cells, we can actually get autoreactive T cells that can actually go ahead and attack our own body, go after our own organs.
Brian Lehrer: As I understand it, Dr. Sakaguchi of Osaka discovered a particular type of T cell called regulatory T cells back in the '90s. That's part of what this Nobel Prize in medicine is for. Can you describe that breakthrough or how he made?
Dr. Daniel Griffin: Really, it's a great story, and hopefully, people will be covering this and hearing more about it, because this was a man, I think I've heard this, swimming against the tide. There was a point in time when we had this idea that the thymus, this organ that most people don't know much about it, not the thyroid, but the thymus, so similar area, just sitting a little bit lower, would do this selection process. You don't want any of these T cells that are going to target you. You want to get rid of them. What we started to realize is that thymus doesn't do a perfect job. It does a great job, and you still would end up with some T cells out there that could react against you.
There was this idea that there were certain, we'll call them traffic cops of the T cells that would keep these autoreactive T cells at bay. Early on, they were called T suppressor cells. It went by very many names. There was this idea that, well, maybe they exist, maybe they don't. Doing research in an area where probably people were saying, "If you're going to make a career, this might not be the gamble you want to make." This, I'll say, brilliant man, Sakaguchi, who had got his MD PhD in Japan, comes over here to the US initially at Hopkins in California.
I bring this up because we still might be the Mecca of science for a while. He does a bit of training, gets some ideas, goes back to Japan, and a few years later realizes that there do seem to be certain traffic cop regulatory T cells, they have a certain flag CD25 on their surface, and these cells tend to actually regulate, tend to protect us. If you give mice T cells without these, they get autoimmune disease. You give the T cells with this CD25, those regulatory cells, and it actually curbs that autoimmunity. Really a shocking, really dense, nerdy paper, but really confirming these T cells, these traffic cops exist.
Brian Lehrer: Starting with Dr. Sakaguchi there, then the two Americans who were working for the same biotech company, is what I've read, figured out which gene mutation was behind a human autoimmune disease.
Dr. Daniel Griffin: It's again an interesting story. This is, again, maybe a plug for why we've got to let scientists do the crazy stuff they do, because sometimes we get these tremendous discoveries, and they're studying this really odd mouse, this scurfy mouse. It has messed-up features. It doesn't live very long. Really, what it does is it has an immune system that is attacking itself. These are back in the primitive days of genetics. They actually figure out that the genetics behind why this mouse has all these problems is a particular disturbance in a gene. This FOXP3. Big long name. FOXP3 is fine for us to use.
They realize that this is affecting these regulatory T cells, which later on, it's all going to come together, and we're going to realize this is the case in these abnormal mice. This is also going to be the master regulator of the T regulatory cells in humans as well.
Brian Lehrer: Dr. Sakaguchi picks up the baton from those scientists and connects what they've discovered to human regulatory T cells.
Dr. Daniel Griffin: Exactly. Really, just a couple years later, he takes that work and then publishes his science paper. That's where this really all comes together. Realizing that if you take these cells that have the functional FOXP3, that they're regulatory, if you put them in, and this is disrupted, then you have the autoimmunity, you put it back in. Actually, using a retrovirus, replace the broken regulator, then the regulatory T cells are working and protecting again. Really tremendous the way all these people are working together to put the pieces of the puzzle here together.
Brian Lehrer: What might these discoveries mean for treatments or cures for human autoimmune diseases? As I understand it, this all hasn't led to treatments yet, but scientists are using this research now to try to develop some.
Dr. Daniel Griffin: It's really true. The way we treat autoimmune diseases right now is really the sledgehammer. We say, "Oh, the immune system is attacking self. We'll shut it down." We try to shut it down. Unfortunately, that really makes our patients susceptible to a lot of my types of diseases, the infectious diseases. The idea here, as we're trying to work to refine this and make this something we can use in patients, is you don't shut down the entire immune system. You regulate it properly. You restore that equilibrium that was supposed to be there in a very selective manner. You don't have to shut the whole thing down.
I should point out, it's not just about autoimmune diseases. Cancer has taken this regulatory T cell and co-opted it for its own use so it can hide from the immune system. We're working on that as well. If you can modulate these regulatory T cells, you can prevent cancers from hiding and allow our immune system to see and go after them and destroy them. Our transplant patients, which is becoming more and more a thing, instead of, again, just shutting down the whole immune system, we're working on the opportunity to modulate it so you can have that kidney replacement, that heart, that lung, whatever it is next. Even things which we don't think of as autoimmune, diabetes, the type 1 diabetes we see in children, which actually is autoimmune. Can we step in and modulate that as well?
Brian Lehrer: Listeners, does anyone have a question, or are we too wonky for you to even form a question for Dr. Daniel Griffin or a comment? Maybe we have listeners who work in studying and treating autoimmune diseases, and you want to weigh in on these discoveries or where you see the particular promise from this field for an application today, call us 212-433-WNYC, 212-433-9692, as we talk about the particulars of this year's Nobel Prize for Medicine.
There are many autoimmune diseases. You just mentioned a few, and from the little I understand, they seem to be grouped by which part of the body the immune system attacks. Is it the skin, like psoriasis? The digestive system as with Crohn's disease? The nervous system with MS? Is that a good way to look at it?
Dr. Daniel Griffin: You're really right. That's the way we've grouped them. The rheumatologists might be the type of doctors who put everything under their umbrella, but you're really right. We group them. The autoimmune diseases that affect the gastrointestinal tract, our gastroenterologists are focused on those. This discovery really points out there's a lot of commonalities here. If your immune system is attacking the gut, probably, your traffic cops are not shutting that down. Same if it's affecting your skin or your brain, or your joints, or anything else. The immunology suggests there's a little bit more of a universal phenomenon going on.
Brian Lehrer: I know from ubiquitous TV ads that many treatments for autoimmune diseases like Crohn's or psoriasis come with warnings that they make you more vulnerable to infection. They're working by suppressing the immune response overall, I guess. Could this research that won the Nobel Prize for Medicine help to avoid that?
Dr. Daniel Griffin: That is really the goal. I think if you think about that study in 2003 in science, that was done where they realized that there was this issue with this master regulator. In those experiments, they replaced the broken part, and then the mice did not have issues. That's our hope, is that we understand what's the broken piece, we fix it, we regulate the immune system. We don't shut it down. We don't leave a person completely vulnerable, scared to go out in public, having to wear a mask, worried they're going to succumb to some infection. We want to restore them to health.
Brian Lehrer: The Nobel Prize for Medicine, I guess we can say with this as an example, isn't for the biggest discovery of the past year. With this, this is the arc of research that, as you've been describing, started in the 1990s and hasn't even produced a treatment yet. It's produced scientific knowledge. What kinds of achievements does the Nobel Prize for Medicine generally recognize?
Dr. Daniel Griffin: Yes, it is really a lifetime achievement award. Even though they pick a particular discovery, it's usually a discovery that's going to influence the field. When we had the mRNA Nobel Prize discovery, it was years of work. Even though we talk about one paper here, one discovery there, it's really someone who's made a fundamental discovery that's allowed science to move forward. It doesn't necessarily have to have given us a vaccine like it did there, but it's the promise, the potential to open up all these doors that are going to allow us to help people. That's what the whole idea of the science Nobel Peace Prizes are about. It's about discoveries that are ultimately going to benefit humanity. That goes back to the history of the Nobel Prizes.
Brian Lehrer: If I may insert one political question at this point, and it may not be the last, but this sounds like basic research, what we call basic research. I'm guessing, tell me if this is wrong, but that this is not the research that's being done by the pharmaceutical companies because they see a relatively short-term or near-term profit in it. It's the research that's funded by government, which we know is being cut now, or am I wrong?
Dr. Daniel Griffin: I think what's great about this Nobel Prize this year is we're actually seeing a little bit of a cooperation going on here. You're correct. I think it's really important to realize that so much of the foundational basic science research does not have a quarterly return. It's a longer vision. It's investment in our society, in our world. Here, I think a couple of these folks were working in private industry when they were allowed to do this. Maybe that's changed in certain ways, but there used to be an investment even at that level in what would be considered more basic science.
Brian Lehrer: Let's take a phone call. Susan in West Orange, you're on WNYC. Susan, hi. You're a nurse, I see.
Susan: I am. Good morning. I'm a home infusion nurse that gives this miraculous T cells in a bottle that came from this basic research to patients who have a variety of autoimmune diseases. I have to say that, for most of them, it's miraculous. Without this basic research, we wouldn't be giving immunoglobulin to people and helping them with their diagnoses. I have a patient I've been giving this to for seven years, who I'm 100% sure would be in a wheelchair right now. She's up walking around and doing things that she never thought she'd be able to do.
It seems like this stuff seems so esoteric, like playing around with these mice and fooling around with these cells in a lab somewhere. What's the application of that? The application is people that are able to actually live their lives.
Brian Lehrer: Susan, thank you. Thank you for your work on the front lines there and relating it to the research that we're talking about that won the Nobel Prize for Medicine yesterday. Another listener writes, Dr. Griffin, "This is so fascinating." They write, "Does it mean we can target cancer? I have pancreatic cancer. I would love to have my T cells altered to attack my mutation."
Dr. Daniel Griffin: That is the hope with a lot of this basic science, is that people may not realize, but I'm going to-- chance to talk about this, is people get cancers on a regular basis. The majority of those our immune system detects at an early stage and gets rid of them. We've already started to try to modulate so that when the cancers try to turn off those T cells, we step in, these checkpoint inhibitors, these new medications. Jimmy Carter, I don't know if people remember Jimmy Carter. He got a melanoma in the back of his eyeball, and his immune system could not see it. We actually used medications that allowed his own T cells to see that melanoma. Within a couple weeks, he was cured.
All this basic science of understanding, regulating T cells, allowing T cells to target cancers, stopping the T cells from targeting us, really are right here where we're starting to see these things actually translate into benefits for human beings that are suffering, that have these issues.
Brian Lehrer: So many of the texts and calls we're getting are from people hoping that this research can lead to something that would help them or someone they care about with all kinds of diseases that are being- or conditions that are being listed. Listener writes, "Is there any hope for eczema sufferers?" Someone else, "I have a form of myositis and take oral immunosuppressant drugs. Could fixing the immune system be used to cure allergies? Can the new information be applied to EBV and other viruses like Lyme disease?"
Another one, "Just diagnosed with diabetes, hoping this science can help." "Does this include mitochondrial disease?" Writes another one. One of those that I read concludes with this question that I'm going to ask you. "How long could this take to come to market for people like me?" Listener writes.
Dr. Daniel Griffin: Yes, a lot of that is up to us. We were really optimistic. It's amazing how much we've learned. It's amazing the momentum, the resources we put into this. People criticize that we put a lot of money into health and science, but I can't see a better place to put that money and resources into improving people's health and well-being. What we're seeing right now is a dismantling of the funding. All this stuff, we're thinking, "Oh, we're just a few years away from those clinical trials," but now we're seeing, we're pushing that away. We're cutting our funding dramatically.
It's this idea that, sorry, if we don't have a cure already, too bad. That has not been the mentality in America. We've got to get back to that hope, that optimism, that funding of progress, the funding of new cures. If you see a physician and you have a problem, we can actually, honestly say, "Okay, we don't have something right now, but we are working on it." As opposed to, "We were working on it, but now we've shut that down to give tax breaks to the billionaires." Is that political, Brian? Was that good?
Brian Lehrer: You're allowed. I have a long history of when I go to the doctor, if they know what I do for a living, I get a lot of, let's say, political opinions, which I love, actually, because doctors tend to be very informed and have interestingly developed opinions. There you go. Let me ask you a follow-up question as it relates to the politics of the Nobel Committee. Do you think the RFK approach to immunology, immunizations, contributed to elevating this specific achievement in medical science at this time?
Dr. Daniel Griffin: I'm sure there's a political aspect to this, not anywhere the same as with the Nobel Peace Prize, which I think is very political. No, I think that this was really an outstanding line of research and brilliant people, and I think they deserve to be recognized. Whatever politics may have been in there, this is an excellent choice, well deserved. I think a long time coming for a recognition of this really groundbreaking, really full of potential discoveries.
Brian Lehrer: Sharon in Westchester, you're on WNYC with Dr. Daniel Griffin. Hi, Sharon.
Sharon: Hi. Thank you for taking my call. First of all, Dr. Griffin, for making such a complex topic understandable. We really appreciate it. My understanding is that autoimmune diseases are more prevalent in women and also increasing worldwide. I'm wondering if these discoveries help us understand those differences in prevalence.
Dr. Daniel Griffin: Great. Thank you for asking that. I think also great for pointing out what you point out here is these diseases disproportionately affect women. Investing in women is investing in this line of research because the people who are going to benefit are going to be the people that have these diseases. As you point out, it's disproportionately going to be women. Yes, whether it's lupus or one of the other diseases, I think that we're going to see the benefits there. Yes, very optimistic. I am optimistic that we're going to turn around the funding, that we're going to get those funds to continue this line of research and get from here to the finish line of something that can actually really help an individual.
Brian Lehrer: Thank you for your question, Sharon. Before you go, let me turn to some of the immunology-related news. I see a headline this morning is that President Trump and the head of the CDC are recommending splitting up the MMR vaccine for kids, measles, mumps, rubella, which is given all at once into three separate vaccines. Measles on one day, mumps another time, rubella another time. Do you have an opinion about that?
Dr. Daniel Griffin: It's untested. This would involve coming up with really brand new products, testing them, getting them through the FDA process. Hundreds of millions of dollars, billions by the time you're down this road. All based on just hunches, feelings, suggestions. It's not a great use of resources. Again, where those resources going to come, or what are they going to come away from?
Here we talk about really exciting science, but are we going to take money away from curing that woman with lupus, curing that individual with a horrible autoimmune skin disease, who's embarrassed to go out without long sleeve shirts and pants, that person who has the scarring of some of the other diseases in autoimmunity? We can go down this road. It doesn't make a lot of sense to be taking the resources away from where they're needed and basically put into some area for someone's agenda, or based upon someone's gut feeling. [crosstalk]
Brian Lehrer: In order to research that. If the concern-- I know parents who are not at all in the RFK anti-vax camp, but who would get concerned when their little ones were up for an MMR vaccine, and might think, well, would there be any harm in splitting them up so there isn't so much going into a kid system all at once? What would they have to research? Could it somehow be bad to split it up?
Dr. Daniel Griffin: I wouldn't suspect it would be bad. Just more needles. That's always been a little bit of their argument, is these kids getting all these injections--
Brian Lehrer: More days where you have to schedule and go to the doctor and get a shot. Right?
Dr. Daniel Griffin: Yes.
Brian Lehrer: What recommendations are you giving your patients on the COVID shot this year? We know how much is changing in terms of federal government recommendations for people who are under 65, let's say, and healthy, or pregnant women in particular. What are you advising your patients?
Dr. Daniel Griffin: Yes, the recent CDC recommendations, and now they've, I guess, codified it. The new acting director has basically said, "Before you get that COVID vaccine, ask your doctor." I guess all the people listening, let me be your doctor for the moment and say across the board, from 6 months all the way up to 100 plus, it is safer to get that COVID vaccine than to not get that COVID vaccine unless you've had an issue, a bad reaction in the past.
Across the board, we're still continuing to make the same science based recommendations, whether it's to prevent you from ending up in the ER, ending up in the hospital, not surviving like the tens of thousands that died last winter, not surviving like the 100 plus children that died last winter from COVID, or all the people that have long COVID, got COVID and just are months and months later not doing better, maybe not able to go to school, maybe not able to hold down a job. That vaccine is still safe, it's effective, and it still is recommended based on all the science and information we have.
Brian Lehrer: It's really been out of the news how many people still die from COVID every year. It's not like it was in 2020 or 2021, but it's become one of the top 10 causes of death in the United States in an ongoing way. Many more people then are killed by flu, for example. Right?
Dr. Daniel Griffin: It is tough. We had 2,000 people a day dying here in New York. It is a very different world now, when we have, we'll say, tens of thousands dying in an entire winter. That's a lot less than 2,000 a day. For your loved one who ends up in the hospital, for your child that dies from COVID, that is still a tragedy. A lot of these deaths are vaccine-preventable.
Brian Lehrer: Dr. Daniel Griffin, MD, PhD, Chief of Infectious Disease Medicine for Island Infectious Diseases on Long Island, a clinical instructor of medicine at Columbia University, president of the group Parasites Without Borders, which sounds like a bad thing, but it's really a good thing. Co-host of the podcast, This Week in Virology, TWiV, as they call it. Thank you for coming on and talking about the Nobel Prize in Medicine and some issues in the news.
Dr. Daniel Griffin: Thank you, Brian, and everyone, be safe.
Copyright © 2025 New York Public Radio. All rights reserved. Visit our website terms of use at www.wnyc.org for further information.
New York Public Radio transcripts are created on a rush deadline, often by contractors. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of New York Public Radio’s programming is the audio record.

