Public Health, Long COVID & Measles
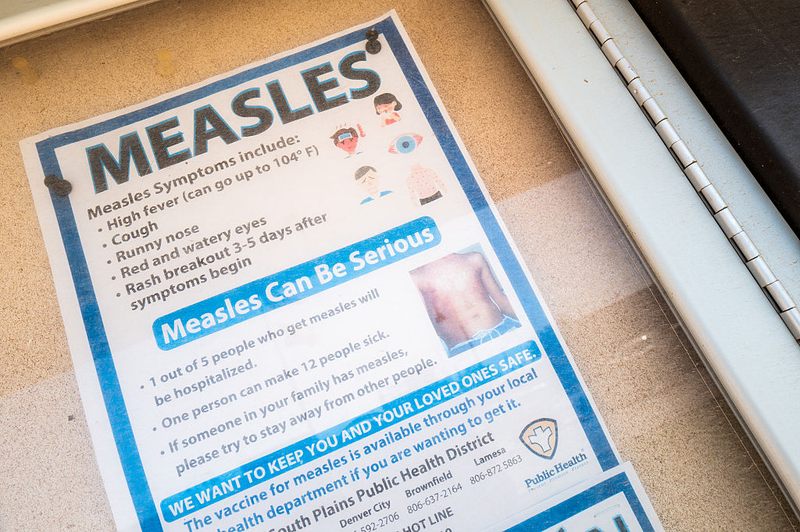
( Brandon Bell / Getty Images )
[music]
Brian Lehrer: It's the Brian Lehrer show on WNYC. Good morning again, everyone. Now, the Health and Climate Tuesday section of the show, as we do every week this week, a couple of challenges to public health. We're facing the surge in measles cases this year, if you haven't heard the extent of that yet, and the ongoing problem of what's called long COVID. Joining us for this is Dr. Daniel Griffin, MD, PhD, Chief of Infectious Disease Medicine for Island Infectious Diseases, the largest physician-owned infectious disease specialist group on Long Island.
Also a clinical instructor of medicine at Columbia University, president of the group Parasites Without Borders, which provides information to medical professionals in countries where parasites are a major cause of disease and co-host of the podcast This Week in Virology, or the acronym TWIV as they like to use. We always learn things when you come on, Dr. Griffin, welcome back to WNYC.
Dr. Daniel Griffin: Thank you, Brian, for having me, and hello to all the listeners.
Brian Lehrer: We want to talk about measles, of course, given the numbers and the issues going on with vaccinations now. Let's start with long COVID. Remind us first, long COVID isn't just one set of symptoms. What's the range you're still seeing?
Dr. Daniel Griffin: Sure. It is unfortunate that we're still seeing new cases of long COVID. What is long COVID? We have a big umbrella term we talked about post-acute sequelae of COVID. These are folks that get COVID, two weeks go by and three weeks go by, four weeks go by, and they're still having issues. Some of those issues are this chronic fatigue type, where they're just not able to think clearly. There's exhaustion, trouble getting up flight of stairs, trouble taking care of the kids, trouble doing work.
Then there's also a whole constellation of other symptoms. You might have a new diagnosis of diabetes out of the blue, you might have cardiovascular problems, you might end up with a stroke. We try to make sure we make a point that COVID is not just a one-and-done for a lot of individuals. You may get through those first two weeks, but then there are all these aftereffects. Brian, I'm glad you're talking about this still because a lot of people don't want us to talk about this. They just want to say COVID is about fatality rates. You live or you die, and that's the end of it. Unfortunately, we're still seeing about 1% of folks end up with ongoing issues, and we just have many month waiting lists for some of our long COVID clinics.
Brian Lehrer: Yes. To your last point, one of the reasons that we invited you today is to promote this special that we're airing tonight at eight o'clock here on WNYC with the public health oriented performance group Theater of War that centers the experience of many people still coping with long COVID, not to mention the challenge to providers like yourself to offer treatments amid all the uncertainty. They talk about feeling left behind by a society wanting to move on from the pandemic, and with limited access to care. I guess that doesn't surprise you.
Dr. Daniel Griffin: No, it doesn't. I appreciate that that special is going to be out there and that people hopefully are going to see that. Hopefully, this is going to remind people to talk about this. I was in the ICU yesterday, and that was a place that had quite a different experience from COVID back in 2020 to what we're seeing now. If you're in a context like that, it seems like it's over. I think a lot of us would like it to be over. For, yes, these people that are either still suffering or now had COVID and are starting to suffer and not getting better, a lot of them are worried they're being left behind.
I have to say, at Columbia, my colleague, Dr. Lawrence Purpura, who is the head of our long COVID, the first funding cut, the first NIH grant that was canceled was his long COVID study. Yes, these people actually have good reason to worry about being left behind because the current climate is that this is something that people don't want to hear about. They want to move on from. We really are fighting hard to keep funding and keep attention on this problem and all the people suffering.
Brian Lehrer: Listeners, we can take calls for Dr. Griffin in this segment on I'm going to call it two and a half topics. It can be on long COVID and your experiences with that, or of people you know. Also, the surge in measles cases in the United States, and anything you want to say, maybe some of you have experience with that, or just ask a question. Long COVID and measles. I say two and a half because also the topic of vaccination in general, which straddles both.
COVID and vaccines, measles and vaccines for Dr. Daniel Griffin, two and a half topics. 212-433-WNYC, 212-433-9692, call or text. In fact, I've read that one thing that seems to make a dent in long COVID is being vaccinated. Is that true? Only in a preventive sense, like you get weaker long COVID if you've been vaccinated, or do vaccines also help people who have long COVID as a treatment?
Dr. Daniel Griffin: I think the data is both, Brian. We saw early on that we're seeing probably 10% to 20% of people getting COVID were not better four weeks later. Once we rolled out the vaccines, that dropped precipitously, probably a 90% drop in long COVID, getting that vaccine ahead of time. Then some other things that we noticed, and this was right after the vaccines came out, and particularly in healthcare workers who were the first to step forward, is we saw about a 60% response to getting vaccinated and either a significant improvement or resolution in symptoms.
Vaccines, great upfront preventing long COVID, preventing post-acute sequelae of COVID, and that's across the board, that's in young kids where we're still seeing about a 1% long COVID. You can really reduce that dramatically by getting vaccinated before the infection. Then some work we've published on with the Mount Sinai and the Yale group where about 60% of people, when they get that vaccine, it actually can really improve their post-COVID symptoms.
Brian Lehrer: Can I ask you in the RFK era, what you're looking for this fall with respect to updated COVID vaccines or the availability of them for different groups?
Dr. Daniel Griffin: Yes, Brian, you could probably imagine, I'm quite worried going forward what's going to happen, and maybe for our listeners to get a little bit of a context here, because I think one of the first things is to remind people that it may not be in the press. A lot of people want to move forward, but COVID is still a significant problem. I'm particularly worried about the children. In April, we had the presentation to American College of Immunization Practices, so the CDC Advisory group basically pointing out that as much as we want to forget about it, we had 153 children die in the last 12 months before that presentation from COVID.
Not with COVID, not incidentally, but very clearly that was what led them to die. The majority, and this is important for listeners here, the majority of those children were completely fine before this happened. That's a parallel that we see with the 256 children that died of influenza this last season, is that this whole idea of only targeting a particular population, the idea that only certain people are at risk, that's not true. It's not true when it comes to COVID and flu, and people not surviving, and children not surviving. Certainly not true when it comes to long COVID.
You have a 1 in 100 chance that when you get COVID 4 weeks later, you may not be better. Vaccines are really our most effective tool at preventing that from happening. I really worried about where we're headed with all this rhetoric about vaccines.
Brian Lehrer: I think we're going to hear a very intense long COVID story from Kim in Brick calling in. Hi, Kim, you're on WNYC.
Kim: Hi. Thank you so much for having me. Yes, I got COVID in January of 2021, so before the vaccine was readily available to the layman, and I was-- When the ambulance drivers arrived at my house, my Pulse Ox was 37. They said I should have been blue, and they couldn't even believe I was responding to questions.
Brian Lehrer: That was your oxygen level, which really should be, like, above 95. Right? It was in the 30s, is what you're saying.
Kim: Yes, absolutely. Yes. If you go to the hospital and your Pulse Ox is in the 80s, they bum rush you. Meanwhile, here I am in the 30s, and they just-- It was a long, long haul after that. I was hospitalized. I got-- Thank goodness, Jersey Shore Medical Hospital had an ECMO bed available for me. ECMO really was up and coming during the pandemic, as far as use for the pandemic. Prior to that, it was used for infants and transplants. That bed becoming available brought my chance of living from 0 to 40%.
Brian Lehrer: By the way, what does ECMO stand for?
Dr. Daniel Griffin: Should I jump in, Kim, with that?
Kim: Oh, please. Please do. You would definitely know better than me. [chuckles]
Dr. Daniel Griffin: It's a machine that basically oxygenates the person's blood for them. You connect-- Yes, the blood comes out, goes through this extracorporeal membrane oxygenation. Don't try to say that fast, but, yes, when your lungs are not working, basically, it's like dialysis for the kidneys. This is oxygenation for the lungs.
Brian Lehrer: Kim, that was the acute or early phase of your COVID 2021, you're saying. You have long COVID of some kind to this day?
Kim: I lost my hearing in my left ear. That was one of the repercussions. I think a lot of people don't realize that can be a repercussion. Like many people lost their smell or their taste. Those nerves all died in my left ear. Unfortunately, those aren't nerves that regenerate. Then I also now sleep with oxygen overnight. I'm very blessed to be able to go without the oxygen during the day, although I do carry an inhaler. I mean, even as you can hear me talking, I'm a very Chatty Cathy. Breathing can be difficult if I'm excited or passionate about something.
After I came home, I actually was on ECMO for about 74 days. It's one of the longest times, especially that early on, that they kept someone on ECMO. Then I was hospitalized from January through-- I left the hospital in May.
Brian Lehrer: Let me ask you how you're being treated, if you're still being treated? I mean, you're certainly talking about at least one long-term permanent effect of your COVID on your hearing. Are you also having other ongoing symptoms that are being treated in the context of this segment?
Kim: I would say, interestingly, I can be very forgetful. I can have lapses of time, things that happened. I actually had gone and gotten a new passport and completely forgotten that I'd ever gotten a new passport. I mean, and that's total-- I said, how could I possibly forget that I filled out this paperwork and mailed it in, and all of the parts that go along with it. It just seems to be that little things like that, they're like glitches, and they happen pretty regularly. It's not something that anybody can fix, per se. I live with that every day.
I try to be present in my actions so that I can hopefully hold onto them for the future. That is definitely something that I'm cognizant of, that I can lose, and because it's scary, I mean, I almost lost all my time. I'm grateful to have it.
Brian Lehrer: Kim, thank you so much for your story. I think it took courage to even call up and tell that on the radio, considering what you've been through. Dr. Griffin, one of the voices that we'll hear in the special tonight at eight o'clock is that of a doctor who talks about that just defining long COVID and diagnosing it is problematic enough. Then there's a lack of treatment options. How do you see the major challenge for doctors with someone like Kim? That's one particular situation. There are various expressions of it.
Dr. Daniel Griffin: I do agree that the first challenge is making the diagnosis. When we've looked at this, there's a lot of individuals who clearly have long COVID issues, post-COVID, and seemingly related to the COVID, they're not getting that diagnosis because doctors are not really trained in how to make that diagnosis. There are a number of educational initiatives, but there's still initiatives and getting put into practice at this point.
The first is actually making that diagnosis, looking at what happened, looking at when they may have gotten COVID, looking at the different symptoms or abnormalities they may have. Now, Kim has this really clear connection right there. I think most doctors are going to be able to say, "Listen, you came in, you were sick, ongoing oxygen requirement, hearing loss. Clearly, this is COVID-related." For a lot of other individuals, it's hard to make that connection. There are not a lot of doctors out there.
I think that's the challenge is getting connected with one of those doctors. As I mentioned, long waiting list to get into a center where someone has the expertise, the confidence to make that diagnosis. Once you make the diagnosis, then you can start going down this road of what are the things that might help? Part of that diagnosis is what type of long COVID might you have? We have this, we call it the ME/CFS, a chronic fatigue, exhaustion, a classic long COVID, where the person is having trouble thinking and unable to participate in activities.
We have pulmonary, where, like we just heard from Kim, ongoing problems with the lungs. There's a cardiovascular, which can have to do with issues with the autonomic nervous system, where your heart is constantly racing. It's always in the upper 90s instead of settling down. There are different types. Then, once you identify those types, there are doctors who are versed in these areas who actually can offer treatment.
I think maybe more importantly, because we're still limited, there's a lot of attempts to do research to look at what may or may not help. Unfortunately, with some of the cuts at the government level, we're really having to reach out and get support from the private sector. In Columbia, for instance, I mentioned with the grant cuts, actually, the Cohen family, Cohen's children, the same family, have stepped in to try to help move things forward.
Brian Lehrer: Let me get one more long COVID story in here from a caller, and then I do want to touch on these measles headlines before we run out of time. Keenan in Crown Heights, you're on WNYC. Hi, Keenan.
Keenan: Hi. Good morning, Brian. Great to be on.
Brian Lehrer: Thank you. Your story starts with a mild case of COVID, I see.
Keenan: Yes. Compared to the previous caller, I barely felt like I had COVID. I really didn't get any initial symptoms and recovered pretty quickly and easily. Now, almost three years on, I still have post-COVID symptoms, including peripheral neuropathy, which is something that is 24/7. My hands and feet are tingling and sometimes in pretty significant pain, and brain fog where I'm feeling slower, which has made it difficult to work sometimes.
Brian Lehrer: How's your treatment plan? Got a good doctor?
Keenan: I've got a few great doctors, but basically they all say we can't be certain that it's COVID-related. Even if it is, there's not much we can do to change anything. It's all being treated symptomatically. It seems like it's just something that I've been left with to deal with.
Brian Lehrer: Keenan, I'm sorry this is happening to you. Another important story. Dr. Griffin, if nothing else, the moral of the story is you don't have to have had an intense case of COVID like the first caller. You can have had a mild case of COVID, like the second caller, and still get long COVID, correct?
Dr. Daniel Griffin: Yes, that is really correct. That's one of the challenges. It's hard to identify ahead of time who's at risk. It's also hard to identify, even during the acute episode, who is going to continue to have issues. We see a disproportionate number of women affected, but we also see men affected. There's different ages that get affected. I think I mentioned that in our adolescents and children, it's probably about 1% or a little bit less. Older folks, the numbers are higher, but then again, it can affect people of all ages.
I love people getting on and sharing these stories, because for a lot of people, that's what it takes. Hearing about that young lady that was in college and now she's at home, debilitated, having trouble going up and down the stairs, the college professor who can't sign their name on a check. Just hearing these stories, I think makes it real for a lot of people. I really applaud the people that called in and shared your stories. That for a lot of people, that's what they need to hear. They need to hear someone tell their story.
Brian Lehrer: Measles. We've seen more cases of measles in the United States this year, from what I've read, than in over 30 years, how worried should we be about 1,288 cases?
Dr. Daniel Griffin: As you say, Brian, there are now more measles cases so far this year, just in-- we're only in July, we're still counting. More cases already so far in 2025 than in any other year since the virus was declared eliminated. That was back 25 years ago in 2000. Unfortunately, we created this perfect storm. This didn't just happen in three months. We've had this gradual decline in vaccine uptake. This scenario was set where we had particular pockets of low vaccination rates. This is a very contagious disease.
We've been warning for a while that eventually something like this would happen. When it does start to happen, we're now 39, they say 39 of the 51 jurisdictions in the US, we have measles cases, we're seeing measles cases, and we already have three deaths in the US. Death up in Canada, a dozen deaths down in Mexico. We should have been worried a while ago. If you're not worried with children dying, then yes, something's wrong.
Brian Lehrer: I read that Canada has more measles cases than the US, and they don't have RFK Jr., so is it from new levels of vaccine refusal there, too?
Dr. Daniel Griffin: Yes, this is really a global problem. Our listeners probably need to be aware of this. It's not just the US. Europe last year had over 100,000 cases of measles. Part of the anti-vaccine stuff started over there, it spread to the US, it spread to all these other places. Now, before RFK took his position in our government, he was working pretty hard. A pretty nice compensation for spreading anti-science and undermining confidence. What really has been one of our most tremendous advances, I mean, vaccination is tremendous. We used to see half a million cases of measles per year in the US. We used to see hundreds of deaths. If things don't turn around, we're headed back in that direction.
Brian Lehrer: Dr. Daniel Griffin, Chief of Infectious Disease Medicine for Island Infectious Diseases on Long Island and a clinical instructor of medicine at Columbia University, President of the group Parasites Without Borders, which sounds like a bad thing, but it's really a good thing. Co-host of the podcast This Week in Virology, where you can catch his weekly clinical updates. Listeners, again, that special on long COVID that we're airing tonight with the theater group Theater of War is at eight o'clock tonight here on WNYC. Dr. Griffin, we always learn when you come on. Thank you very much.
Dr. Daniel Griffin: Oh, thank you, Brian. Everyone, be safe.
Copyright © 2025 New York Public Radio. All rights reserved. Visit our website terms of use at www.wnyc.org for further information.
New York Public Radio transcripts are created on a rush deadline, often by contractors. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of New York Public Radio’s programming is the audio record.

